The Virta Clinical Trial Outcomes at 1 Year Demonstrate Improved Non-alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes

Nonalcoholic fatty liver disease (NAFLD) is an increasingly common cause of liver cirrhosis¹,², and is projected to soon become the major cause of liver transplantation¹,²,³. The direct medical cost of managing NAFLD and its associated complications are estimated over $100 billion per year in the United States and projected to further increase⁴. There are at least 84 million people in the United States living with either type 2 diabetes or prediabetes causing NAFLD, and a substantial number of these patients will progress to non-alcoholic steatohepatitis (NASH) and liver fibrosis⁵. Yet routine screening and management of nonalcoholic fatty liver disease (NAFLD) in patients with type 2 diabetes is often overlooked, either because doctors are unaware of effective non-invasive diagnostic techniques, or because current treatment strategies are marginally effective⁵,⁶.
Rather than expensive imaging or an invasive needle-biopsy to get liver histology, a simple blood test for liver enzymes can be used to calculate liver fat and fibrosis scores, providing an alternative for the diagnosis of liver fat and ruling out advanced fibrosis⁷,⁸. In our recently published 1-year results, we reported a significant decrease in all three major liver enzymes, alanine aminotransaminase (ALT), aspartate aminotransaminase (AST) and alkaline phosphatase (ALP) in the patients receiving Virta’s continuous care intervention⁹. Similar improvements in liver enzymes were not observed in the group of usual care (UC) patients receiving standard treatment for type 2 diabetes in this study⁹. Using the enzyme changes in these patients with type 2 diabetes, we utilized these recently validated equations to score their risk of increased liver fat (steatosis) and fibrosis.
Key liver function results from the Virta Health—IU Health Diabetes Clinical Trial
Table 1 shows the changes in key liver enzymes, c-reactive protein (a biomarker of inflammation), the calculated non-invasive NAFLD scores, weight, and HbA1c. For each marker, we show the change between baseline and 1 year as a percent. Patients receiving the continuous care intervention from Virta showed significant reductions in liver enzymes, fat score, fibrosis score, along with weight and inflammation). In contrast, there were no significant improvements in these biomarkers in the usual care control group.
Table 1 Liver-related Outcomes in the Virta Clinical Trial at One Year
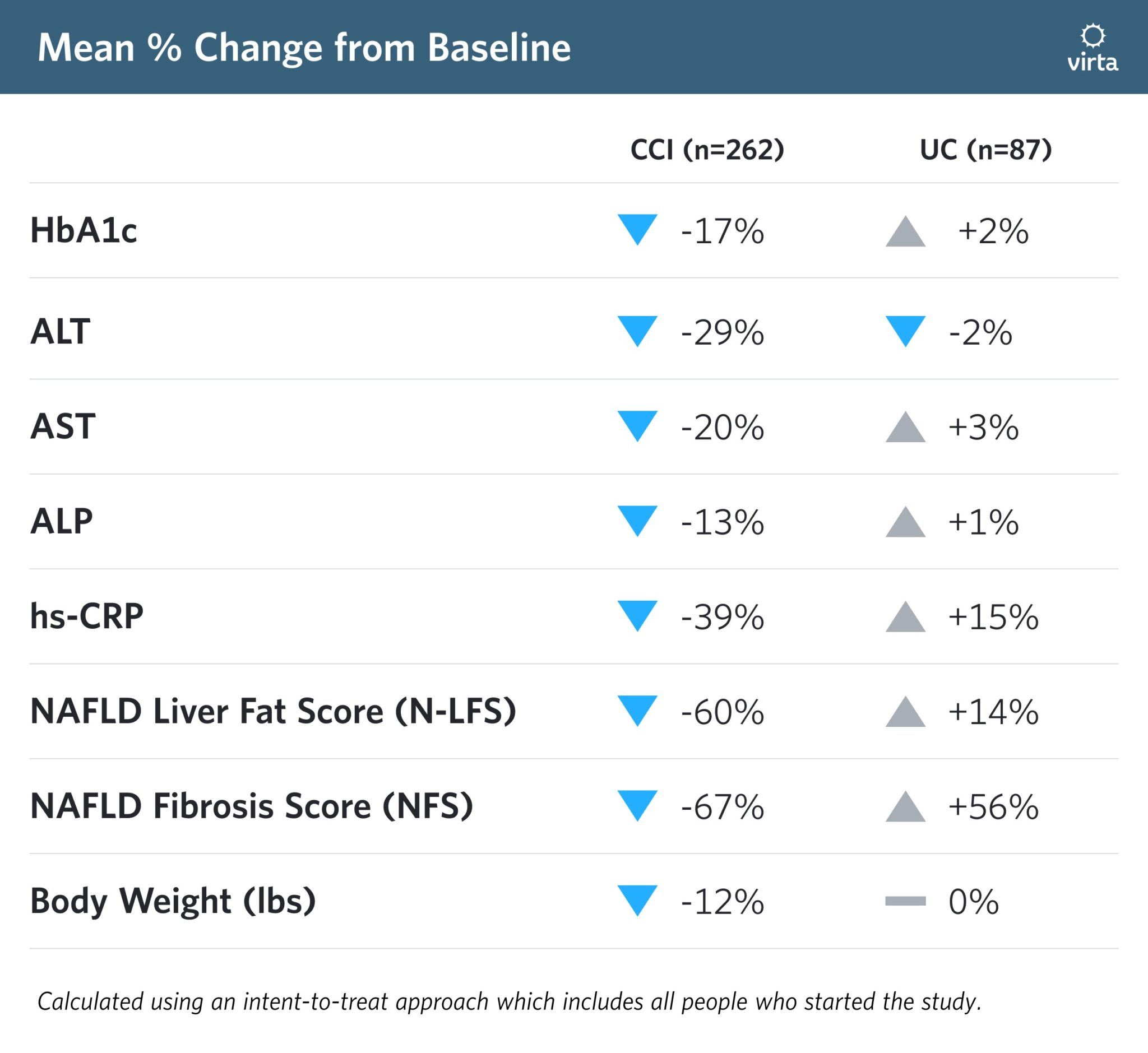
These results show that the Virta continuous care intervention substantially improved liver- and NAFLD-related outcomes in patients with type 2 diabetes, while at the same time reducing body weight and improving blood glucose control. Although improving glycemic control is recommended for patients with NAFLD and NASH, there is limited evidence showing that maintaining glycemic control using anti-diabetic medications improves liver histology and fibrosis⁵,⁶,¹⁰. The continuous care intervention is not only effective at improving and sustaining glycemic control while discontinuing the majority of anti-diabetes medications⁹; it also improves NAFLD and fibrosis in patients with type 2 diabetes.
How a well-formulated ketogenic diet reduces liver fat and improves liver health
The most effective current treatments for NAFLD and NASH focus on weight loss and exercise. Sustained weight loss has been reported to improve liver enzymes, fat content and liver histology⁷,⁸,¹¹. Weight loss of at least 3–5% is recommended to improve liver fat content or steatosis⁷,⁸. A greater weight loss of 7–10% appears necessary to show histopathological improvement of NASH and fibrosis⁷,⁸. However most patients with type 2 diabetes, especially those taking glucose lowering medications, find even these modest weight loss thresholds hard to achieve and sustain.
In contrast to a standard calorie-restricted diet, a well-formulated ketogenic diet dramatically reduces the body’s need for insulin, which in turn allows the body to accelerate its rate of fat burning. In particular, fat stored in the liver is used to make ketones (using up to 50 grams of liver fat per day), which allow the liver to mobilize accumulated fat and thus reduce steatosis. Together, these increases in fat use lead to weight loss without prescribing a calorie-restricted diet. Thus, 54% of the clinical trial patients receiving the Virta treatment had > 10% weight loss, while 79% of the patients had > 5% weight loss at one year.
While it is tempting to attribute improved liver health to weight loss, in truth these are associations; whereas the actual cause of improved liver health is likely some combination of carbohydrate restriction, reduced blood insulin, and accelerated fat oxidation. Inflammation also has a strong association with liver injury, and a well-formulated ketogenic diet has strong anti-inflammatory effects as shown in this study⁹,¹³. But whatever the mechanism of this improved liver function with the Virta CCI, patients achieving greater weight loss (the majority of the patients) had a higher resolution of liver enzymes, steatosis and fibrosis.
Implications of the liver findings
These data from liver-related markers and scores demonstrate improvements at one year not only in type 2 diabetes outcomes but also in the resolution of comorbidities NAFLD and fibrosis. These findings were demonstrated using liver fat and fibrosis scores that have been proven to correlate well with results from imaging and histological assessment, techniques that could be used in future studies to directly assess liver status in selected populations.
Terminology and Notes:
NAFLD - Nonalcoholic fatty liver disease: a liver condition characterized by excess fat accumulation in the liver in absence of heavy alcohol consumption.
There are two types of NAFLD:
1. Steatosis or simple fatty liver: More than 5% of the weight of the liver tissue is composed of stored fat.
Factoid: It takes just 75 grams of stored fat for the liver to reach this 5% fat threshold. Severe steatosis may reach fat levels 2-3 times this amount. But if the liver uses 50 grams of fat per day to make ketones, a liver suffering from steatosis could use this pathway to get rid of its excess fat in just 2-6 days.
2. NASH - Nonalcoholic steatohepatitis: Liver disease with injury, inflammation and cell death; in addition to steatosis
Liver fibrosis - Severe NASH with liver injury and scarring
The information we provide at virtahealth.com and blog.virtahealth.com is not medical advice, nor is it intended to replace a consultation with a medical professional. Please inform your physician of any changes you make to your diet or lifestyle and discuss these changes with them. If you have questions or concerns about any medical conditions you may have, please contact your physician.
Visit our research page to learn more about our clinical trial and research on type 2 diabetes and other chronic metabolic conditions.
This blog is intended for informational purposes only and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or any advice relating to your health. View full disclaimer
Are you living with type 2 diabetes, prediabetes, or unwanted weight?

- Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease- Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016; 64(1): 73-84.
- Younossi ZM, Marchesini G, Pinto-Cortez H, Petta S. Epidemiology of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis: implications for liver transplantation. Transplantation 2018; doi: 10.1097/TP 0000000000000000002484.
- Younossi ZM, Blissett D, Blissett R, Henry L, Stepanova M, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology 2016; 64: 1577-1586.
- Bril F, Cusi K. Management of nonalcoholic fatty liver disease in patients with type 2 diabetes: a call to action. Diabetes Care 2017; 40: 419-430
- Tilg H, Moschen AR, Roden M. NAFLD and diabetes mellitus. Nat Rev Gastroenterol Hepatol 2017; 14(1): 32-42
- Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, et al. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology 2012; 55(6): 2005-2023.
- European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016; 64(6): 1388-1402.
- Hallberg SJ, McKenzie AL, Williams PT, Bhanpuri NH, Peters AL, et al. Effectiveness and safety of a novel care model for the management of type 2 diabetes at 1 year: am open-label, non-randomized, controlled study. Diabetes Ther 2018;9: 583-612.
- Raschi E, Mazzotti A, Poluzzi E, De Ponti F, Marchesini G. Pharmacotherapy of type 2 diabetes in patients with chronic liver disease: focus on nonalcoholic fatty liver disease. Expert Opin Pharmacother 2018; doi.10.1080/14656566.2018.1531126.
- Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology 2015; 149: 367-378.
- Raschi E, Mazzotti A, Poluzzi E, De Ponti F, Marchesini G. Pharmacotherapy of type 2 diabetes in patients with chronic liver disease: focus on nonalcoholic fatty liver disease. Expert Opin Pharmacother 2018; doi.10.1080/14656566.2018.1531126.
- Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology 2015; 149: 367-378.
- Phinney S, Bailey B, Volek J. Inflammation, nutritional ketosis, and keto-immune modulation: new insights into how virta can reverse type 2 diabetes. https://blog.virtahealth.com/inflammation-ketosis-diabetes.