
Reversing Type 2 Diabetes: An Evidence-Based Guide
An evidence-based guide to type 2 diabetes reversal options
in the U.S. is suffering
from diabetes or prediabetes¹
In the U.S., about 49% of the adult population is suffering from type 2 diabetes or prediabetes1. Type 2 diabetes happens when the body’s cells don’t respond to insulin correctly. This causes glucose (sugar) to build up in the blood, instead of being converted into energy in the cells. Elevated blood sugar is associated with a host of problems, and if left unchecked, can lead to type 2 diabetes.
Type 2 diabetes can be a devastating disease, and is often mistakenly regarded as progressive, meaning that it will only get worse over time. However, multiple clinical trials have shown that type 2 diabetes can be reversed.
What is diabetes reversal?
Diabetes reversal, as defined by an international panel of experts, is the process of returning glucose levels below those diagnostic of diabetes2.
Virta recognizes this definition while also adding some nuance. We consider diabetes reversed when someone achieves an A1c below 6.5%, without requiring diabetes medications other than metformin. Metformin is excluded from reversal criteria because it is not diabetes-specific—many patients choose to stay on this medication for reasons other than blood sugar control.
So what does all of this actually mean? Because type 2 diabetes is diagnosed based on elevated blood sugar, if your blood sugar remains normal without the use of diabetes-specific medications (other than metformin) and you no longer meet the diagnostic criteria, you have reversed your type 2 diabetes.
For more information
Read our blog post on Reversing Type 2 Diabetes with Nutritional KetosisWhat is A1c?
How type 2 diabetes can be reversed
There are three forms of treatment that are demonstrated to reverse type 2 diabetes:
Bariatric surgery
Bariatric surgery (also called metabolic surgery) can sometimes reverse type 2 diabetes3, but it is expensive, can have major side effects, and often loses its effectiveness after a few years4. Because it’s an invasive procedure, it’s usually not considered a “first line treatment” for reversing diabetes.
Very low calorie diets
Very low calorie diets (also called semi-starvation diets) can also lead to rapid weight loss and diabetes reversal5. However, these diets can only be followed for a few months, after which weight maintenance and continued diabetes control are difficult6. Very low calorie diets are usually medically supervised and require an intake of less than 800 calories per day.
Very low carbohydrate diets
The third treatment is a very-low carbohydrate diet. Carbohydrate restriction (and specifically very low carbohydrate nutrition therapy such as well-formulated ketogenic diets) can quickly result in lower blood sugar, less reliance on diabetes medications, weight loss, and can reduce hunger7. Many of these improvements can be sustained, too8. Usually, very low carbohydrate diets are defined by an intake less than 50g of total carbohydrates per day.
Reversal vs. remission vs. cure
The terms “reversal” and “cure” mean very different things. Type 2 diabetes can be “reversed” but not “cured” because the disease will continue to progress if long-term behavior change is not maintained.
“Remission” is another term that’s often used interchangeably with “reversal.” While the definitions are slightly different—the goal is the same—to control diabetes and return blood sugar to below diagnostic thresholds.
Remission happens when blood sugar returns to sub-diabetes levels, and stays that way for more than three months without any diabetes medication2.
Can type 2 diabetes be reversed naturally?
Type 2 diabetes can be reversed naturally—or without medications and surgery—with diet and lifestyle changes. One of the most-studied eating patterns for reducing A1c and medication dependence is carbohydrate restriction11.Reversing diabetes may not be possible for everyone—for example, people who are more recently diagnosed may be more likely to achieve reversal naturally6. But even in the absence of reversal, adherence to some of the natural methods for achieving it may still lead to an overall reduction in A1c, less reliance on diabetes medications, and more benefits like:8
- Weight loss
- Improvements in cardiovascular health, and markers of kidney and liver function
- Increased control over eating
Reverse your diabetes naturally—see if you're eligible for Virta Health.
What is nutritional ketosis and why does it work for reversing type 2 diabetes?
Why does carbohydrate restriction work so well for people with type 2 diabetes? Because of something called “nutritional ketosis.” Nutritional ketosis is a natural metabolic state that allows your body to burn fat and ketones rather than carbohydrates as its primary fuel source.
At the heart of nutritional ketosis are 'ketones', or small molecules that are made from fat in the liver. Ketones provide energy to fuel important organs like the brain, heart, and muscles. They also play a role in reducing oxidative stress (free radicals) and inflammation, both of which are key underlying contributors of type 2 diabetes.
Given that ketones are both fuel and a metabolic regulator, nutritional ketosis is one of the most effective treatment options for sustainably reversing type 2 diabetes. It is clinically proven to reduce blood sugar (as measured by HbA1c), improve insulin sensitivity, and reduce inflammation. Since type 2 diabetes is a disease of high blood sugar, insulin resistance, and inflammation, nutritional ketosis is an effective diabetes reversal tool because it can improve all three.
Entering a state of nutritional ketosis requires changing what you eat. To learn more about nutritional ketosis and how it can help reverse type 2 diabetes, read more here.

The safety of diabetes reversal
Diabetes reversal treatment should always be done under medical supervision. When your blood sugar is no longer chronically elevated, blood sugar-lowering medications may no longer be necessary. So medications that rapidly reduce blood sugar need to be removed, such as insulin and sulfonylureas, sometimes in as little as 2 days to 2 weeks. Blood pressure often improves, too, meaning blood pressure medications may also need to be eliminated. Other medications like SGLT-2 inhibitors, DPP-4 inhibitors, GLP-1 receptor agonists, and metformin may be removed as long as normal blood sugar is maintained.
Any dietary, lifestyle or other change that brings blood sugar back into normal range needs to be closely monitored by a medical provider in order to ensure that medications are safely deprescribed.
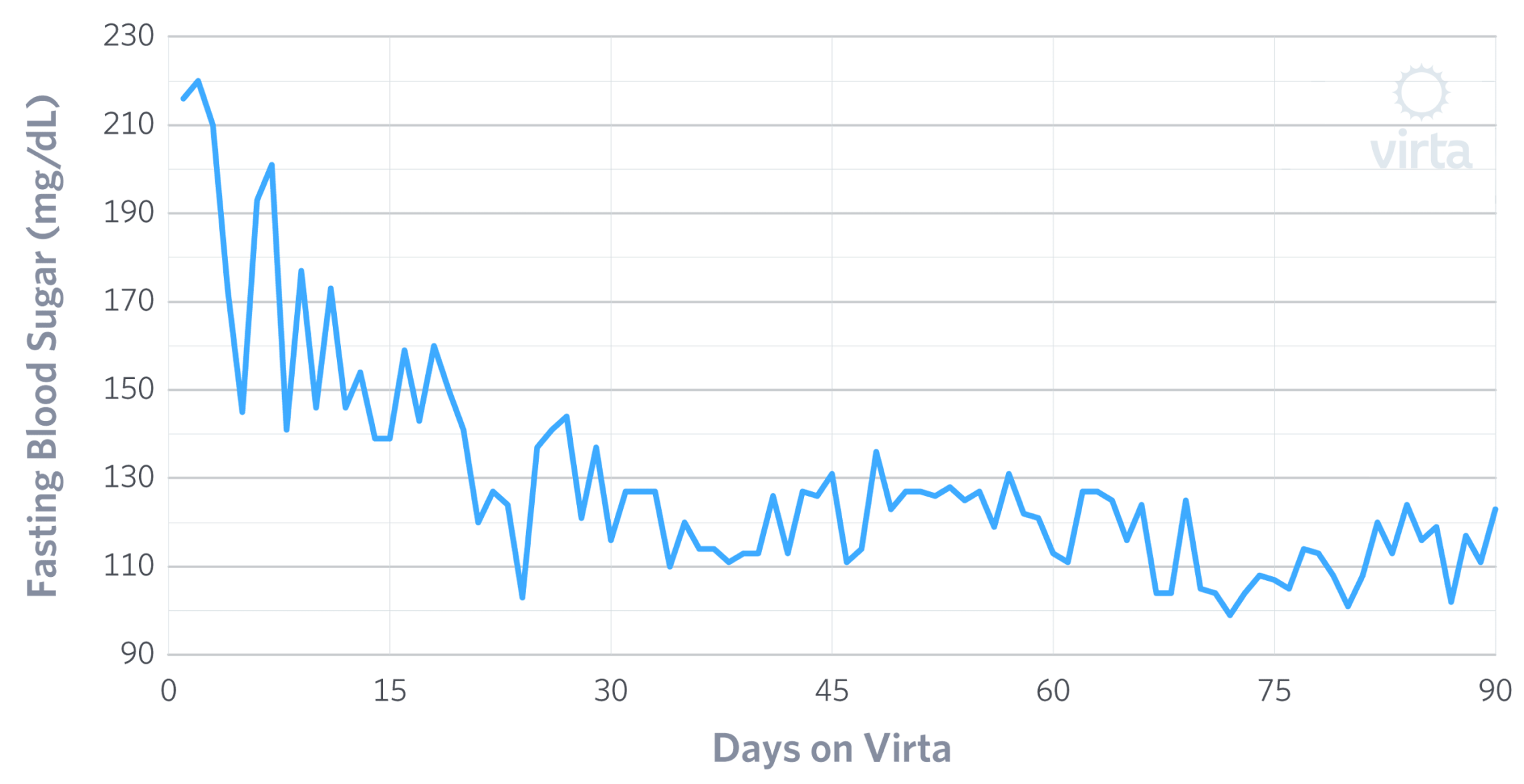
Fasting Blood Glucose improvements
(Sample Virta patient)
Making reversal last
Another question around reversal, especially for diet and lifestyle interventions, is sustainability. Is reversal realistic long-term?
In a traditional doctor-patient setting, where visits to medical providers happen a few times per year, sustained diabetes reversal may be difficult. Without proper support, lifestyle changes can be hard to start and maintain.
That’s where the telehealth revolution comes into play. For example, Virta provides “continuous remote care,” which gives patients around-the-clock support from health coaches and medical providers. This team also monitors biomarkers (things like weight and blood sugar) and makes recommendations for reducing medications in near real-time. This type of model, which is radically different from current models of infrequent or “episodic” care, makes reversal a real option. Technology enables the care delivery needed to not only reverse diabetes, but also sustain it.
When your blood sugar is no longer chronically elevated, these blood-sugar-lowering medications are no longer necessary. An ongoing study has shown that sustained nutritional ketosis can lead to the removal of these medications10. Medications that rapidly reduce blood sugar need to be removed first, such as insulin and sulfonylureas, sometimes in as little as 2 days to 2 weeks. Other medications like SGLT-2 inhibitors, DPP-4 inhibitors, GLP-1 receptor agonists, and metformin can be removed as long as you maintain normal blood sugar.
If you are on diabetes or blood pressure medications, Virta highly recommends that you get medical supervision before making any dietary changes.
In closing
While diabetes is typically thought of as a chronic condition, it is possible for many people with type 2 diabetes to reverse the progression of their disease. And with the right treatment and support, it can be done naturally without surgery or medication.
See if you qualify for for diabetes reversal treatment at no additional cost
Frequently Asked Questions
- National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States. Accessed at: https://www.cdc.gov/diabetes/data/statistics-report/index.html.
- Riddle MC, Cefalu WT, Evans PH et al. Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes. Diabetes Care 1 October 2021; 44 (10): 2438–2444. https://doi.org/10.2337/dci21-0034.
- Robert M, Ferrand-Gaillard C, Disse E, et al. Predictive factors of type 2 diabetes remission 1 year after bariatric surgery: impact of surgical techniques. Obes Surg. 2013 Jun;23(6):770-5. doi: 10.1007/s11695-013-0868-4. PMID: 23355293.
- Courcoulas AP, Gallagher JW, Neiberg RH, et al. Bariatric Surgery vs Lifestyle Intervention for Diabetes Treatment: 5-Year Outcomes From a Randomized Trial. J Clin Endocrinol Metab. 2020 Mar 1;105(3):866–76. doi: 10.1210/clinem/dgaa006. PMID: 31917447; PMCID: PMC7032894.
- Lean ME, Leslie WS, Barnes AC, Brosnahan N, et al. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet 2019 May 01.https://doi.org/10.1016/S2213-8587(19)30068-3
- Gregg EW, Chen H, Wagenknecht LE, et al. Association of an Intensive Lifestyle Intervention With Remission of Type 2 Diabetes. JAMA. 2012;308(23):2489–2496. doi:10.1001/jama.2012.67929.
- McKenzie AL, Hallberg SJ, Creighton BC, et al. A Novel Intervention Including Individualized Nutritional Recommendations Reduces Hemoglobin A1c Level, Medication Use, and Weight in Type 2 Diabetes. JMIR Diabetes. 2017 Mar 7;2(1):e5. doi: 10.2196/diabetes.6981. PMID: 30291062; PMCID: PMC6238887.
- Athinarayanan SJ, Adams RN, Hallberg SJ, et al. Long-Term Effects of a Novel Continuous Remote Care Intervention Including Nutritional Ketosis for the Management of Type 2 Diabetes: A 2-year Non-randomized Clinical Trial. Frontiers in Endocrinology. 2019; 10:348. doi: 10.3389/fendo.2019.00348.
- Boden G, Sargrad K, Homko C, et al. Effect of a Low-Carbohydrate Diet on Appetite, Blood Glucose Levels, and Insulin Resistance in Obese Patients with Type 2 Diabetes. Ann Intern Med. 2005. https://doi.org/10.7326/0003-4819-142-6-200503150-00006
- Volk BM, McKenzie AL, Athinarayanan SJ, et al. A Population Shift in Meeting Glycemic Targets Following Five Years of a Very-Low-Carbohydrate Intervention (VLCI) and Continuous Remote Care (CRC) . Diabetes 1 June 2022; 71 (Supplement_1): 1176–P. https://doi.org/10.2337/db22-1176-P.
- Evert AB, Dennison M, Gardner CD, et al. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Diabetes Care 1 May 2019; 42 (5): 731–754. https://doi.org/10.2337/dci19-0014.

